In late 2019, UTHealth School of Biomedical Informatics (SBMI) Dean, Professor, and the Glassell Family Foundation Distinguished Chair in Informatics Excellence Jiajie Zhang, PhD, wrote a blog post that made this analogy; “AI is to Medicine Today What the X-ray was to Medicine a Century Ago.” Since writing that blog, the health care industry has been turned upside down by the strain of the COVID-19 pandemic. However, technological advancement did not stop during the pandemic – a large part of it received a boost because of the pandemic. Over the past one to two years, AI applications have been developed and utilized at a much higher speed and at a much larger scale to help improve and transform how medical care is provided.
In his latest presentation on medical AI, Dean Zhang provides a deeper dive into what he meant when he made the analogy “AI is to Medicine Today What the X-ray was to Medicine a Century Ago.” He also discusses the significance of medical AI in both historical and economic contexts and uses concrete examples to demonstrate how medical AI is fundamentally transforming medicine and healthcare.
To access the slide deck of Dean Zhang’s presentation, click here. For the transcript of the presentation in pdf, click here.
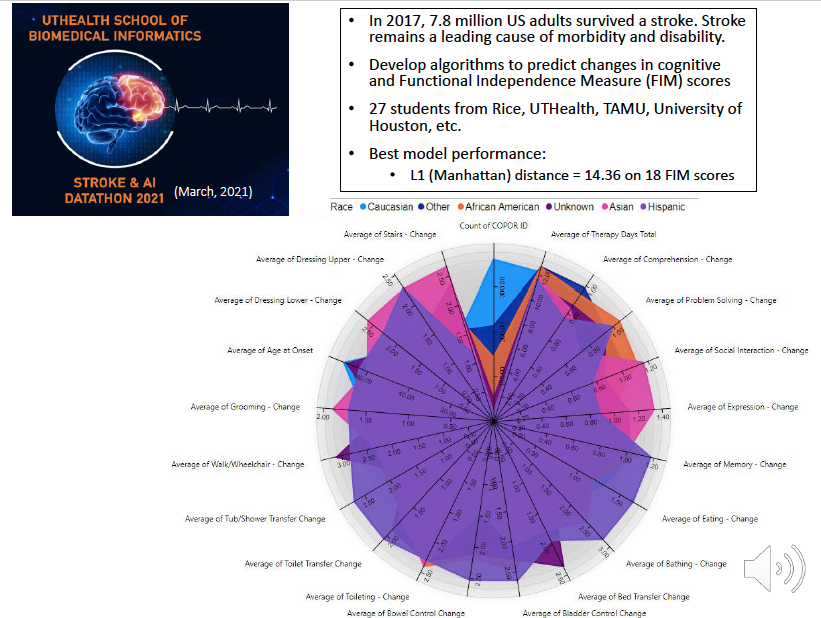
Slide 18:
In the most recent Datathon we hosted last month, the students were asked to build a machine learning model to predict how well a stroke patient recovers over time.
Specifically, the students need to develop algorithms to predict changes in cognitive and Functional Independence Measure scores. Again the models the students developed performed well.
Solving a real world medical problem with real patient data within 24 hours; by undergraduate and graduate students, some of whom only learned the basics from an intro to machine learning course.
This is exciting; but think about it, it is also kind of scaring. Having a model that makes good predictions, however, does not mean that makes an impact on the patients.
Slide 19:
Medical AI is still very hard.
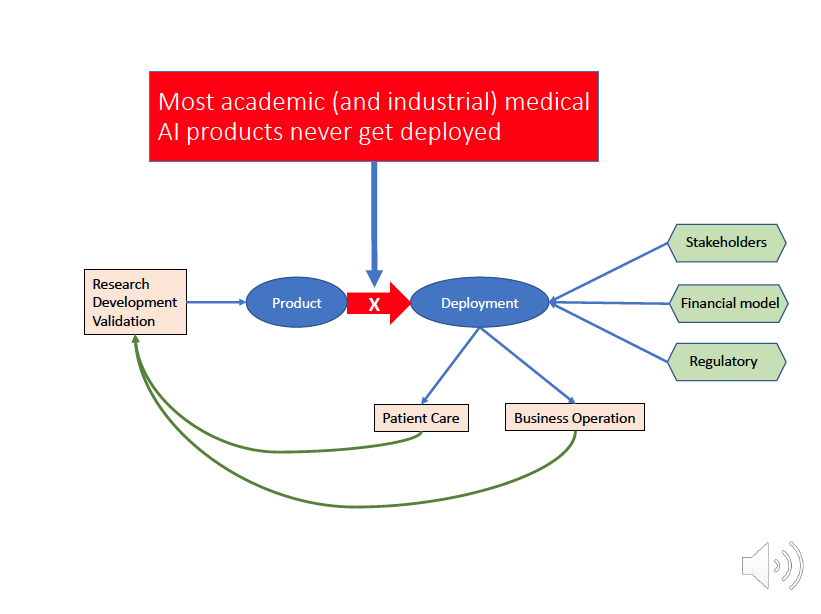
Slide 20:
Most academic (and industrial) medical AI products never get deployed. There are many reasons why.
After research and development, and after validation, both internally and externally, a medical AI product is ready for testing in the real clinical setting. However, getting the product into the production environment is one challenge. How to get it into the clinician's workflow is another, bigger challenge.
What are the clinical and business utilities of the product? How to get it go through the regulatory process both internally and externally, such as FDA? How to keep the product updated with new data, modified with new algorithms? What about patient safety concerns? The list goes on and on. Let us look at a real use case to understand the complexity of getting medical AI product into the clinical setting.
Slide 21:
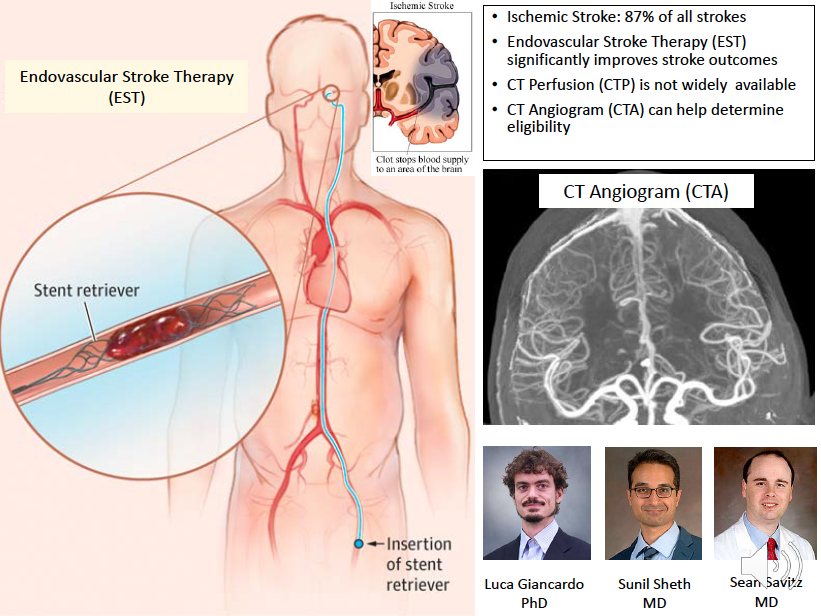
This case is about CT imaging for stroke.
Slide 22:
There are two types of stroke: ischemic stroke that is the blockage of the blood vessel and the hemorrhagic stroke that is the breakable of the blood vessel. Ischemic stroke accounts for 87% of stoke and there is a therapy that can save a patient’s life. This therapy is called endovascular stroke therapy, or EST, which is to insert a stent retriever from the groin all the way to the brain to remove the blood clot. CT Perfusion, or CTP, is the definitive guide to determine whether a patient is eligible for this procedure. CTP is an advanced procedure that is not widely available at smaller facilities. A relative simpler technique called CT Angiogram, or CTA, is more widely available but it is typically not good enough to determine EST eligibility. Dr. Giancardo, in collaboration with neurologists Dr. Sheth and Dr. Sean Savitz, developed a machine learning model that can use CT Angiogram to do what CT Perfusions’ job.
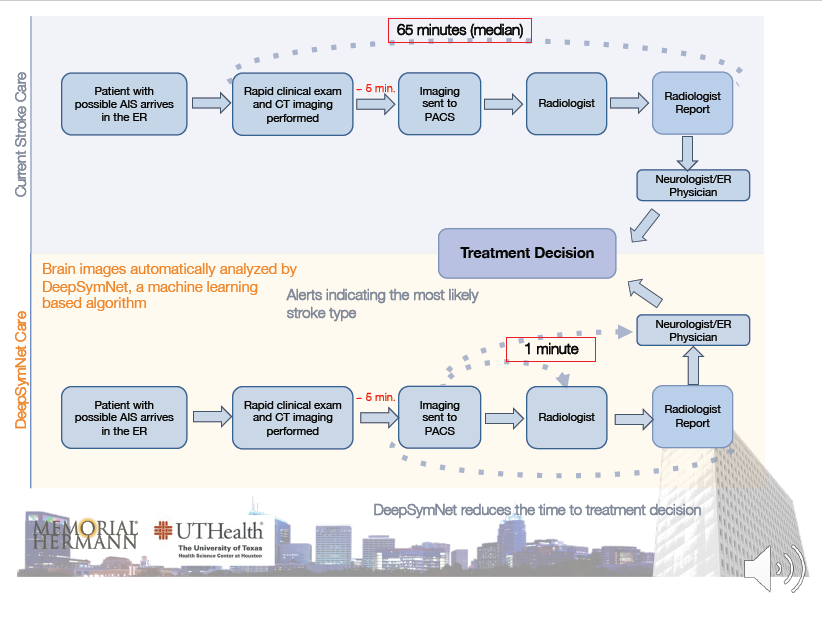
Slide 23:
They successfully developed a CT Angiogram based AI system called DeepSymNet, which has a very good performance level. This system reduced the time from patient’s ER arrival to treatment decision dramatically because the AI system only takes 1 minute to read the CT and send the report to the physicians for treatment decision.
Slide 24:
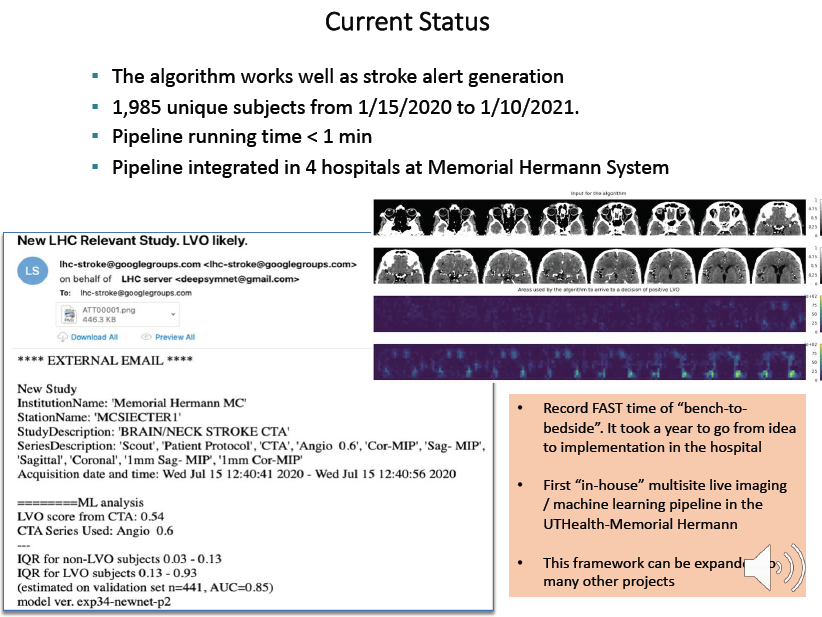
The system generates an alert after image analysis by the AI system and sent it to the stroke team by email that has an EST eligibility score along with the CT images.
The development and implementation of this system recorded a very fast “bench-to-bedside” time. It took a year to go from idea to implementation in the hospital and this is very fast.
The pipeline for this system is now integrated in 4 hospitals and it is functioning in near real time. As we can see, this AI pipeline sends alert by email which is outside of the EHR platform. Getting this system integrated into the EHR platform and the workflow of the clinicians will be next step, which is non-trivial and may well be the major barrier to its wide adoption.
Slide 25:
A technically capable AI product needs to be deeply integrated into the clinical environment and it needs to show it’s clinical, operational, and financial utilities before it can be widely adopted to generate meaningful impact on patient care. This deep integration requires a lot more than AI algorithms. It requires an entire discipline called biomedical informatics; and it requires an insider’s job, that is, researchers and clinicians in healthcare institution.
Slide 26:
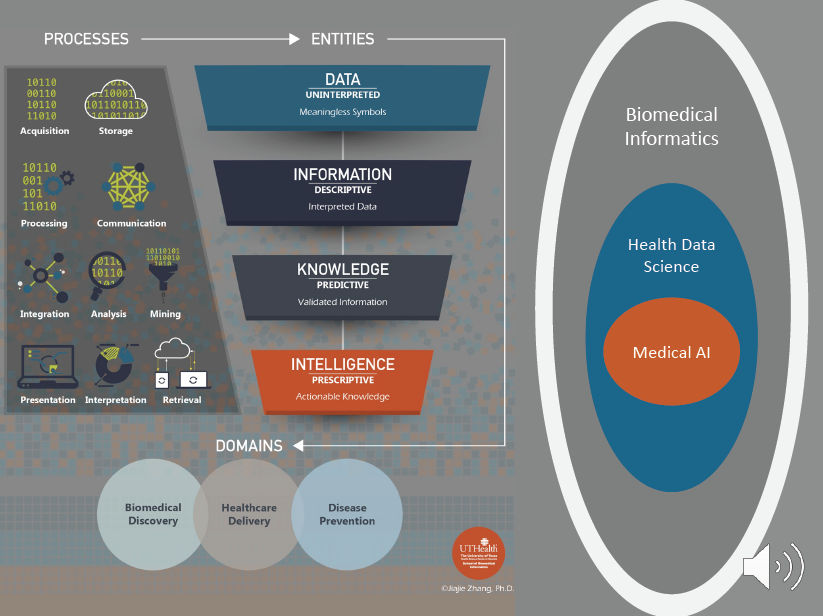
Biomedical Informatics studies the acquisition, storage, communication, processing, integration, analysis, mining, retrieval, interpretation, and presentation of data and determines how to transform data, which are meaningless symbols, to information, which are interpreted data, to knowledge, which are validated information, and to intelligence, which are actionable knowledge, with the aim of solving problems in disease prevention, healthcare delivery, and biomedical discovery.
Biomedical informatics covers the entire spectrum of biological scales—from small molecules, genes, proteins, and cells, to tissues and organs, to individuals and populations. Biomedical informatics is a highly interdisciplinary field focused on collaborations with partners in clinical practice (e.g., medicine, nursing, dentistry, pharmacy); the biomedical sciences; public and community health; computer science and engineering; mathematics and statistics; cognitive science; social and behavioral sciences; healthcare management; and health IT policy and law.
Data Science for medicine is a subfield of Biomedical Informatics; it focuses on all aspects of data for disease prevention, healthcare delivery, and biomedical discovery. Medical AI is in turn a subfield of Health Data Science, and it focuses on machine learning, pattern recognition, computational phenotyping, and predictive modeling.
Our School of Biomedical Informatics at the University of Texas Health Science Center at Houston is the only free-standing school among 70 or so such programs in the nation, and it is one of the largest internationally.
The AI Revolution promises to be an exciting era. With virtually unlimited potential, medical AI is rapidly evolving to produce ever greater numbers of increasingly advanced clinical applications that will dramatically improve patient care, disease prevention, and biomedical discovery. We are proud to be a leader in medical AI. Health data science, and biomedical informatics. It’s great to be part of that transformation!
Slide 27:
Thank you for your time. Hope you enjoyed this presentation. If you want to learn more about medical AI, health data science, biomedical informatics, or the education programs at our school, you can reach me by email or follow me in social media. Thank you.